A simple, clear guide for expecting families.

Gestational diabetes (also called GDM) is a type of diabetes that first appears during pregnancy. It happens when your body cannot use sugar (glucose) the way it should. This can lead to high blood sugar, which can affect both you and your baby.
The good news?
Most people with gestational diabetes have healthy pregnancies with the right care, screening, and nutrition.
Here is what the latest research from the American Diabetes Association (ADA) and ACOG recommends.
💗 If You Are Diagnosed: What Happens Next?
If you are diagnosed with GDM, your care team will help you create a plan.
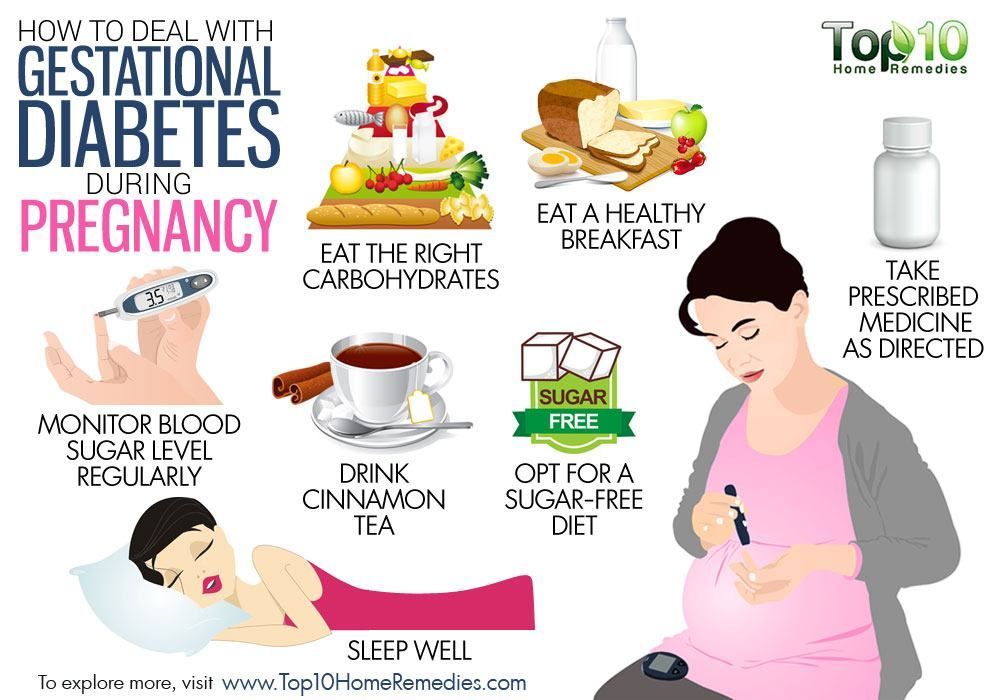
This usually includes:
- Meeting with a diabetes educator or dietitian
- Learning how to check your blood sugar
- Making nutrition changes
- Adding gentle exercise
- Sometimes taking insulin or medication
Most people manage GDM with nutrition and lifestyle changes alone.
💗 Nutrition Guidelines
Healthy eating is one of the most important ways to manage gestational diabetes.
The ADA and ACOG recommend:
🥗 1. Eat Regular, Balanced Meals
Try to eat 3 small meals + 2–3 snacks a day.
This helps keep your blood sugar steady.
🍞 2. Choose Complex Carbs Instead of Simple Carbs
Better choices (slow-release energy):
- Whole grains
- Brown rice
- Quinoa
- Beans and lentils
- Whole-grain pasta
- Sweet potatoes
Limit simple carbs:
- White bread
- White rice
- Candy and sweets
- Soda
- Juice
🍳 3. Add Protein to Every Meal
This helps balance blood sugar.
Healthy proteins:
- Eggs
- Chicken
- Turkey
- Fish (low mercury)
- Beans
- Tofu
- Greek yogurt
🥑 4. Include Healthy Fats
These make meals more filling.
Healthy fats:
- Avocado
- Nuts
- Seeds
- Olive oil
- Nut butters
🚰 5. Drink Plenty of Water
Avoid sugary drinks. Choose:
- Water
- Sparkling water
- Unsweetened tea
🚶♀️ 6. Try Gentle Exercise
Movement helps lower blood sugar naturally.
Good options:
- Walking
- Prenatal yoga
- Swimming
ACOG recommends 150 minutes a week of moderate activity if approved by your doctor.
💗 Blood Sugar Goals
Your provider may ask you to check your blood sugar.
Typical targets:
- Fasting (before breakfast): under 95 mg/dL
- 1 hour after meals: under 140 mg/dL
- 2 hours after meals: under 120 mg/dL
Your personal targets may vary depending on your pregnancy.
💗 Will Gestational Diabetes Go Away?
For most people, yes.
Blood sugar usually returns to normal after birth.
However, you should have a blood sugar test 6–12 weeks postpartum, because some people develop type 2 diabetes later.
Staying active and eating healthy after pregnancy lowers this risk.
💗 Final Thoughts
Gestational diabetes can feel scary, but remember:
- You did not cause it
- You didn’t do anything wrong
- With good care, most pregnancies go very well
- You have many tools to help keep you and your baby healthy
You are not alone. Your care team is here to support you every step of the way.